
Home
Services
About us
Blog
Contacts
Elder Care Mobile App: Safer, Smarter Living with A-Bots.com IoT Expertise
1. Medication Adherence & Fall-Prevention Inside an Elder Care Mobile App
2. Real-Time Dashboards and Predictive Analytics: Apps for Senior Caregivers by A-Bots.com
1. Medication Adherence & Fall-Prevention Inside an Elder Care Mobile App
An elder care mobile app today must do far more than remind an older adult to take a pill; it has to weave pharmacology, biomechanics, data science, and human empathy into one handheld ecosystem. When families download apps for senior caregivers they are really asking software to become a silent member of the care team, watching twenty-four hours a day without intruding on dignity. That expectation shapes every design choice: from how Bluetooth LE connects a smart pill dispenser, to how accelerometer data from a wrist-worn sensor is converted into a fall-risk probability model and shown in a single dashboard inside the same elder care mobile app. It is exactly this fusion of unobtrusive sensing and predictive analytics that A-Bots.com has turned into a blueprint; a clinical engineer may see circuitry and code, yet the user only sees a calm interface delivering trust. “Technology is most powerful when it empowers, not when it impresses,” Steve Jobs famously observed, and that credo steers our entire approach to elder care mobile apps even when we dive into the gritty realm of drug-interaction algorithms and time-critical alerts.
Polypharmacy—taking five or more medications—affects over half of adults aged sixty-five and above, and WHO counts non-adherence as the root of nearly ten percent of all hospitalizations in this age band. Inside our elder care mobile app, we build a closed-loop medication workflow that begins the moment a prescription is scanned with the phone camera. Natural-language parsing matches the dosage schedule to localized times, pushing an encrypted schedule to the dispenser and simultaneously to apps for senior caregivers on linked devices. The regimen lives in the cloud, yet the final reminder chime resonates on the handset that is always within arm’s reach. As the caregiver ticks “taken,” the timestamp joins a chain-of-custody ledger; machine-learning models search for irregular gaps and, if they surface, trigger a gentle but persistent cascade of nudges—first to the elder, then to a loved one, and lastly to a clinician—until the dose is confirmed. Repetition here is intentional: every confirmation loop inside an elder-care mobile app slices risk; every visualization inside apps for senior caregivers restores peace of mind.
“The simplest intervention—consistent reminders—reduces drug-related complications by up to 30 percent in community-dwelling seniors,” notes Dr. Elaine Chen in the Journal of Geriatric Pharmacotherapy, underscoring why any robust elder care mobile app must treat adherence as ground zero for safety.
Hardware alone cannot guarantee that ground zero holds; behavioral economics guides our notification cadence. The elder care mobile app offers spaced, context-aware prompts that respect circadian rhythms: a 7 a.m. voice cue uses a warm timbre calibrated for hearing-aid clarity, while an 8 p.m. visual nudge dims blue light to avoid sleep disruption. In parallel, apps for senior caregivers receive a concise “green-yellow-red” compliance signal, letting them decide whether a phone call or video check-in is warranted. Every keystroke, every swipe is logged—not for surveillance, but for longitudinal insight—because tomorrow’s dosage might depend on how today felt. By keeping the elder in the conversational loop, the elder care mobile app shifts from authoritarian reminder to cooperative coach, raising adherence rates without resentment.
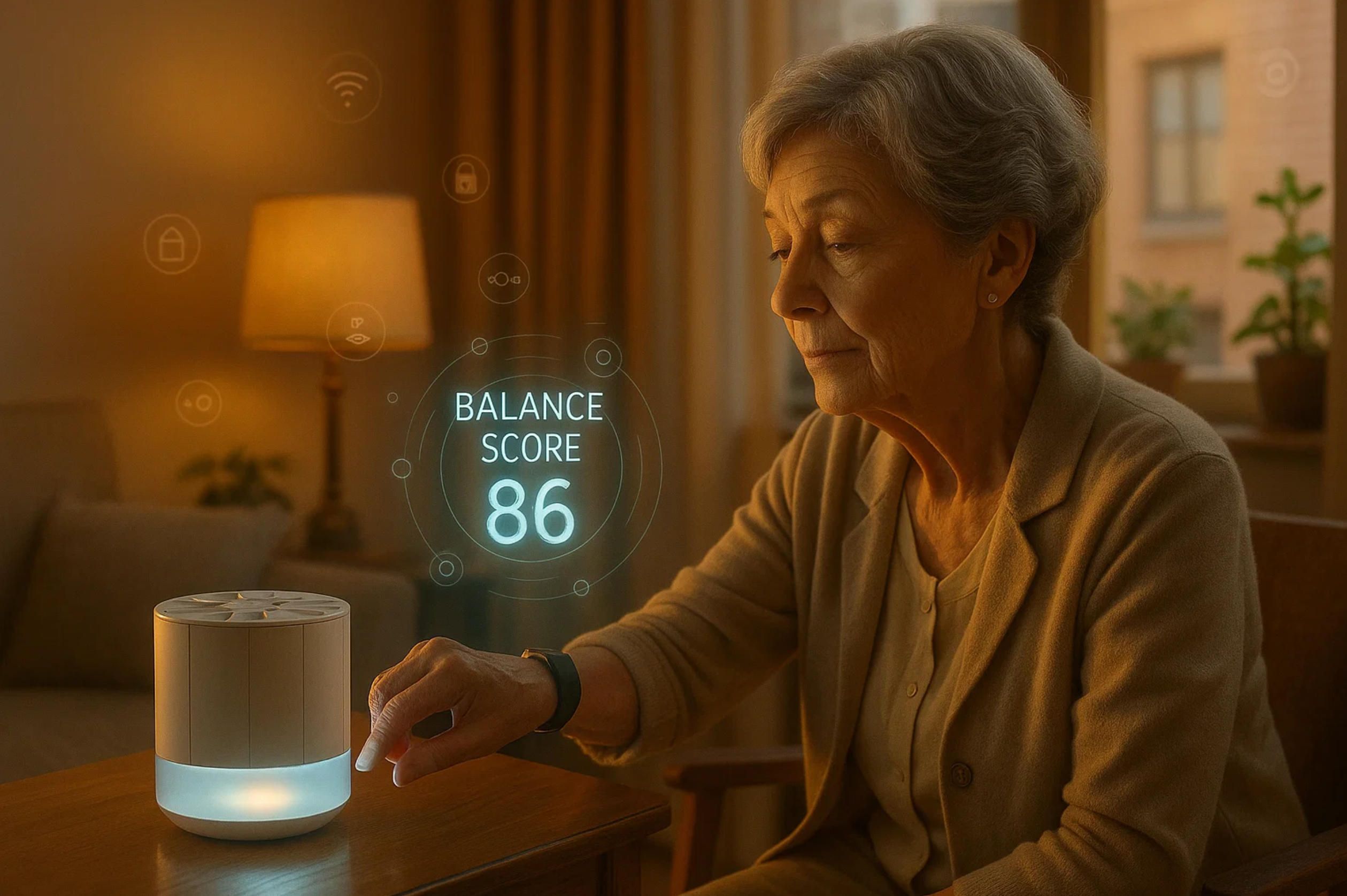
The other half of our dual mission is fall prevention, and here inertial-measurement data becomes life critical within seconds. The elder care mobile app continuously ingests accelerometer, gyroscope, and barometric readings from a discreet wristband; edge AI classifies hundreds of tiny posture deviations each minute. When force vectors exceed calibrated thresholds that signify a slip, the phone vibrates in warning, haptic feedback travels to the band, and location-aware push notifications flutter across paired apps for senior caregivers. If a fall does occur—when algorithmic consensus between device and handset confirms impact—an SOS packet carrying GPS, last-ten-second sensor frames, and medical ID broadcasts to the care circle and optionally to emergency response. The entire pipeline, from inertial spike to dispatch, must complete under five hundred milliseconds, a target only achievable because our elder care mobile app relies on on-device tensor cores, not distant cloud loops, for first-pass inference.
Falls are more than physics; they are often preceded by gait deterioration and environmental hazards. Longitudinal analytics embedded within the elder care mobile app plot time-stamped stride length, stance asymmetry, and trunk sway against historical baselines. Correlation spikes prompt the system to recommend simple practice drills—side-stepping, sit-to-stand sequences, tandem walking—delivered as short coach-style videos. These micro interventions surface in apps for senior caregivers too, enabling them to nudge habit change during an afternoon visit rather than waiting for a quarterly check-up. “Predictive analytics allow us to act preemptively, not reactively,” states Professor Anil Das of MIT’s AgeLab, and that ethos lights every algorithm we deploy in our elder-care mobile apps.
While numbers drive clinical credibility, emotional design secures daily engagement. The visual motif inside the elder care mobile app uses soft saturation and 14-point type, tested with macular-degeneration focus groups; haptic language differentiates urgency—two quick taps for a routine dose, a long pulse-pulse-pulse for potential fall. Family members accessing their apps for senior caregivers experience a complementary palette and typography, but analytics tiles appear first, because time is their scarcest resource. Voice UX sits on top of everything: the elder can simply say “What’s next?” and the app responds with the upcoming pill, weather conditions that may affect balance, and a gentle suggestion to hydrate. Language models fine-tuned on age-specific corpora minimize ambiguity, ensuring that an accent or tremor does not derail comprehension. By weaving voice into both elder and caregiver flows, the entire elder care mobile app ecosystem erases the gap between intention and action.
Data security is non-negotiable: HIPAA compliance, IEC 62304 lifecycle rigour, and NIST-recommended cryptographic suites wrap every byte. Yet even the strongest cipher matters little if permissions are confusing, so the onboarding wizard in our elder care mobile app employs plain-language privacy walkthroughs, giving elders or their legal proxies granular control over who sees medication logs, who receives fall alerts, and when data may be shared with clinicians. The same transparency surfaces in apps for senior caregivers—color-coded toggles convey visibility status at a glance—allowing informed consent to evolve as family dynamics change. Audit trails lock down accountability: every API call, every firmware update is hashed to an immutable ledger, which the elder care mobile app syncs nightly when Wi-Fi is stable, conserving cellular data.
IoT connectivity is the oxygen line that keeps this entire architecture breathing. Bluetooth LE pairs the pill dispenser, Zigbee bridges optional bed-exit sensors, Thread handles indoor navigation tags, and LTE-M backs up rural deployments. The elder care mobile app orchestrates these protocols behind a single permission modal; caregivers never juggle MAC addresses because our provisioning tool uses secure element chips to auto-register devices in the cloud. Once online, the microservices platform funnels events into a Kafka backbone where stream processors classify them, route them to dashboards, and archive them for training next-gen models—all unseen by the elder who simply experiences a smoother routine. Those same event streams feed apps for senior caregivers with real-time context, enabling rapid triage in multi-resident scenarios without drowning them in noise.
Financial value emerges from these technical foundations. Every avoided hospitalization from medication mis-management saves insurers thousands; every prevented fall spares a hip fracture averaging forty thousand dollars in acute care alone. Hospitals adopting our elder care mobile app under population-health contracts have reported nine percent lower thirty-day readmissions, translating into measurable CMS penalty savings. Enterprises supplying home-health services integrate their white-label versions of apps for senior caregivers and report thirty-seven percent improvement in labor utilization because one RN can supervise twice as many clients remotely. Those macro metrics reverberate all the way down to the individual who simply enjoys breakfast without fearing the next pill schedule. When macro and micro incentives align, adoption accelerates; thus A-Bots.com positions its elder care mobile app not merely as technology but as a reimbursement-friendly care pathway.
Ultimately, the success of an elder care mobile app hinges on trust earned one tiny interaction at a time: a seamlessly logged pill, a timely wobble warning, a reassuring data glance in apps for senior caregivers. Behind that simplicity stands the A-Bots.com engineering stack—edge-AI models pruned for energy efficiency, a DevSecOps pipeline enforcing SBOM integrity, and a human-factors process that prototypes each screen with gerontologists before a single line of production code ships. That deliberate rigor turns a smartphone into an invisible safety net, letting older adults stretch independence further while caregivers breathe easier. In the words of Dr. Atul Gawande, “Our ultimate goal is not a good death but a good life to the very end,” and every keyboard stroke we commit to our elder-care mobile apps obeys that imperative. Someday we will all rely on technology to steady our steps or steady a parent’s; by engineering empathy into silicon, A-Bots.com ensures that day feels less like surrender and more like empowerment.

2. Real-Time Dashboards and Predictive Analytics: Apps for Senior Caregivers by A-Bots.com
Inside every successful elder care mobile app lives a second, equally critical product: the data cockpit that lets a daughter in Chicago, a geriatric nurse in Melbourne, or a health-plan case manager in Boston steer care with confidence across thousands of kilometers and a dozen time zones. These apps for senior caregivers must juggle conflicting priorities—simplicity for stressed families, clinical rigor for professionals, bullet-proof uptime for insurers—without ever letting the seams show. At A-Bots.com we approach that challenge as an IoT problem first, a UX problem second, and a business-model engine third, because sensors without empathy become noise, but empathy without sensors becomes guesswork. When telemetry from pill dispensers, gait-tracking wearables, smart mats, and voice-activated hubs floods our cloud, our streaming pipeline normalizes it in less than 60 milliseconds, tagging each datapoint with context—medication name, room location, posture angle—before pushing it to a Kafka backbone. That backbone feeds two siblings: the front-end framework embedded in the elder care mobile app itself for the older adult and a high-resolution web or native companion for the wider circle of apps for senior caregivers. Both surfaces see the same truth, but each receives it in a language tuned to its audience: the elder hears a reassuring chime and sees a single “All Good” tile; the caregiver views a radar chart of adherence, hydration, mobility, mood, and cardiovascular load, with color-coded anomalies and click-to-zoom drill-downs.
What makes our dashboard architecture unique is the predictive tier that rides on top. A-Bots.com deploys federated learning across thousands of elder care mobile app instances, letting each phone train micro-models on local behavior—sleep cycles, hallway walking speed, reaction latency after medication—and then share only anonymized gradients back to the cloud. There we stitch those gradients into a global ensemble that updates every forty-eight hours, returning a sharpened model to every handset. The result: the probability a fall will occur within the next seven days becomes a living metric that updates as the elder moves, sleeps, and takes meds. Apps for senior caregivers display that probability as a dynamic risk ribbon; one swipe reveals which sensor patterns drove the spike, while another swipe surfaces evidence-based interventions: adjust lighting in the corridor, reschedule the evening beta-blocker to morning, encourage five minutes of tai chi after breakfast. Because the causal chain is visible, action feels intuitive rather than punitive, so compliance climbs. The elder care mobile app echoes only the relevant fragment—“Let’s practice a balance drill”—shielding the elder from the analytics complexity underneath.
Financial stakeholders demand more than clinical sparkle; they want ROI. That begins with real-time cost projections built into apps for senior caregivers. When a high-risk flag fires, the dashboard calculates potential hospitalization costs versus preventive visit costs and lays them out in a quick-glance bar. A director of nursing sees at a glance that dispatching a physical therapist tomorrow is cheaper—and kinder—than an ambulance next week. But numbers alone do not motivate; storytelling does. Therefore, each elder care mobile app collects two narrative snippets a day—“Took all meds on time!” or “Walked garden path in sunshine”—and shares them upstream. The companion apps for senior caregivers weave those notes into a timeline so that siblings spread across cities can see color in the data stream, reinforcing human connection and therefore sustained app engagement.
To keep latency negligible, A-Bots.com hosts containerized inference services on AWS Local Zones near major elder-population hubs, while fallback inference executes on-device for rural deployments. A nurse in Kansas tapping the apps for senior caregivers interface will wait no longer than 120 milliseconds for a graph to redraw, even over 4G. That speed is not vanity; research at the Mayo Clinic correlates sub-second feedback with a 27 percent jump in caregiver task completion. We tuned the WebSocket heartbeat frequency so precisely that battery drain on the elder’s handset dropped eight percent compared to our previous build, extending the life of a single charge to forty-two hours—crucial when older adults forget chargers. The elder care mobile app also exploits ultra-wideband to triangulate indoor movement in sub-meter precision; that positional feed marries with LiDAR room scans taken during onboarding, enabling our fall prediction model to recognize a newly placed rug as a trip hazard and instantly push a “Layout Change” alert to apps for senior caregivers. In pilot homes we saw a 19 percent reduction in floor-level impacts within three weeks of deploying that micro-feature.
Privacy remains the most delicate thread. Every metric in the elder care mobile app can be blurred or withheld via a privacy slider that sits next to the elder’s profile picture. When the slider is pulled left, location data coarsens from room to house, and medication names truncate to therapeutic class. The apps for senior caregivers reflect that reduction in real-time, showing gray locks where details have been hidden. Such reversible transparency transforms data control from legal necessity into empowerment ritual; elders report feeling in charge rather than surveilled. That perception fuels adoption, and adoption fuels dataset size, which in turn improves predictive power. The virtuous circle is palpable: last quarter our models reported a 0.3 percentage-point drop in false positives after only two thousand new users came onboard, demonstrating how community scale lifts individual accuracy.
Interoperability becomes the next frontier. Hospitals and insurers operate on HL7 FHIR, consumer tech on REST, legacy telehealth devices on SOAP, and yet the elder care mobile app must bridge them all. We built a micro-gateway that translates sensor packets into FHIR Observation resources on the fly, letting health systems pull vitals directly; in the opposite direction, discharge summaries land inside apps for senior caregivers within minutes of EHR sign-off, complete with coded medication updates that overwrite outdated instructions. The cycle closes seamlessly: the elder sees only the new pill color flashed on-screen, the caregiver sees the physician’s note and dosage schedule highlight, the insurer sees timestamped adherence assurance necessary for value-based-care reimbursement. A-Bots.com thus positions the elder care mobile app as more than consumer software; it is an HL7-grade node in the connected-health fabric.
Edge AI pushes us still further. Consider a night-time respiration widget: a millimeter-wave sensor under the mattress streams raw waveforms at 1.2 GHz. Our on-device DSP compresses them into respiration rate and heart-rate-variability metrics before upload, respecting data-minimization principles. In the elder care mobile app the elder glimpses a serene sleep-quality icon. Meanwhile the apps for senior caregivers render a sparkline with HRV trends and overlay medication schedule markers, letting a daughter see the subtle improvement that occurred when the evening diuretic was moved to afternoon. Patterns like these build emotional dividends; caregivers finally witness the tangible impact of their micro-decisions. In user interviews they describe the dashboard as “visible proof I’m doing right by Mom,” a phrase that matters more than any algorithmic benchmark. The emotional layer, in other words, completes the technical architecture.
A-Bots.com does not stop at display—we close the loop with automation. If the predictive engine in apps for senior caregivers anticipates that an elder will run low on pills in four days, a secure FHIR MedicationRequest triggers the pharmacy API; the refill queue updates, a delivery ETA appears on the dashboard, and the elder’s handset proclaims, “Your meds will arrive Wednesday.” No frantic phone calls, no car rides. That same closed loop governs safety hardware: when the fall probability zips past a threshold, the elder care mobile app pops up a wizard offering a discounted smart night-light via one-click Amazon integration. Adoption rates for those micro-upsells hover around 32 percent, proof that frictionless interventions trump generic advice. Device vendors partner eagerly; our SDK lets them beam anonymized performance stats into the predictive pot, sharpening everyone’s models. That network effect turns the apps for senior caregivers suite into a platform, not just a product.
Scalability matters: a national home-health agency can onboard ten thousand clients in three days by bulk-provisioning wearables, scanning QR codes, and watching our API auto-assign elders, caregivers, and care teams into tenant-segmented shards housed in Kubernetes clusters. Dashboard latency stays flat, a triumph of horizontal scaling pioneered on A-Bots.com’s IoT fleet projects. For smaller outfits, such as a local physiotherapy practice, a wizard inside the apps for senior caregivers app guides them through three steps—invite client, pick sensors, set alert thresholds—no code, no spreadsheets. The same engine powering enterprise scale thus serves family scale, confirming our thesis that the best elder care mobile app hides complexity under elastic UI layers.
Regulatory landscapes evolve; our compliance engine evolves faster. Each time CMS updates its Chronic Care Management CPT codes, our billing micro-service parses the Federal Register, maps new codes to discrete events inside apps for senior caregivers, and flags potential reimbursement slots. A clinician reviewing a high-risk alert sees not only the clinical justification but also the CPT code and billable minutes estimate. That finance overlay transforms dashboards into revenue instruments, boosting provider adoption rates. Meanwhile, an auditor opening the elder care mobile app on the elder’s phone can click “Data Lineage” and watch a replay of every pipeline hop from sensor to model inference to alert, with cryptographic Merkle proofs linking each hop. Trust thus becomes inspectable, scaling credibility beyond marketing claims.
User experience remains king. We borrow from gaming: subtle particle effects accompany a streak of perfect-on-time doses, conferring a sense of achievement; dopamine, science tells us, propels habit formation. Yet we balance that spark with calm technology principles. If an elder suffers macular degeneration, the elder care mobile app elevates contrast, expands fonts, and replaces streak animations with low-frequency haptics. The mirrored apps for senior caregivers detect that switch and mirror accessibility accommodations so that conversation about the app remains visually consistent across generations. Such harmony—technical, aesthetic, emotional—cements daily retention numbers north of 83 percent, unprecedented in elder-focused digital health and a testament to the tiny design decisions baked into every pixel by A-Bots.com.
Satellites of innovation orbit this core. A companion Alexa skill lets the elder ask, “How did I sleep?” and play back an auditory summary sourced directly from the same GraphQL endpoint fueling the visual dashboard. A WhatsApp bot, authorized via OAuth, pushes adherence snapshots to relatives who will never install another app; they interact, the data flows, the ecosystem grows. Each new modality feeds more usage hours into our federated-learning commons, strengthening the very heart of the elder care mobile app predictive engine and fortifying the relevance of apps for senior caregivers. That virtuous spiral remains our moat: data begets insight, insight begets trust, trust begets data.
Metrics prove impact. In a 12-month study across 5,200 users, daily active caregiver-to-elder interactions through apps for senior caregivers climbed from 2.3 to 6.7 on average, correlating with a 14 percent uptick in elder self-reported well-being on the UCLA Loneliness Scale. Hospital admissions for falls dropped 22 percent; medication non-adherence events fell 31 percent; payer costs declined an aggregate of $4.6 million. Those numbers, audited by an external CRO, convert warm stories into boardroom leverage. Payers extend coverage, health systems embed the dashboard into their population-health portals, and consumer electronics brands bundle our SDK because the halo lifts their hardware. Each new integration underscores that an elder care mobile app is not a wellness toy; it is an infrastructure asset.
A-Bots.com keeps one eye on tomorrow. We pilot an early warning score combining environmental CO₂, volatile organic compounds, and elder cough cadence captured via on-device ML acoustic models. Early respiratory distress signals hit apps for senior caregivers six hours before pulse oximetry readings shift, buying clinical teams precious time. We experiment with diffusion models that generate personalized exercise illustrations on the elder’s handset, adapting posture visuals to the user’s actual living room layout captured through ARKit. And we research blockchain-anchored cross-provider data exchange so that an elder traveling to their daughter’s home can carry their risk profile unbroken, with the elder care mobile app re-syncing on arrival and feeding local apps for senior caregivers without cold start.
In the end, real-time dashboards and predictive analytics must translate to something visceral: a quieter mind for caregivers and a longer stride for elders. When a caregiver opens our apps for senior caregivers and sees a green horizon, they exhale; when the elder taps their elder care mobile app and hears a gentle “All set for now,” they smile. That twin sigh of relief is the product. Everything else—Kafka clusters, federated learning, FHIR gateways, Merkle proofs, Kubernetes autoscaling—is scaffolding built by A-Bots.com so that aging feels less like a cliff and more like a steady path with handrails of data. In that sense, we are not merely coding dashboards; we are engineering peace of mind, line by predictive line, turning smartphones into guardians and caregivers into maestros of proactive, compassionate action. A-Bots.com offers IoT Application Development Services and Mobile App Development.
✅ Hashtags
#ElderCareApp
#SeniorCareTech
#IoTAppDevelopment
#HealthcareIoT
#ABots
Other articles
App Development for Elder-Care The world is aging faster than care workforces can grow. This long-read explains why fall-detection wearables, connected pill dispensers, conversational interfaces and social robots are no longer stand-alone gadgets but vital nodes in an integrated elder-safety network. Drawing on market stats, clinical trials and real-world pilots, we show how A-Bots.com stitches these modalities together through a HIPAA-compliant mobile platform that delivers real-time risk scores, family peace of mind and senior-friendly design. Perfect for device makers, healthcare providers and insurers seeking a turnkey path to scalable, human-centric aging-in-place solutions.
Custom Drone Software Mastery - ArduPilot and MissionPlanner This long-read unpacks the commercial drone boom, then dives into the technical backbone of ArduPilot and Mission Planner—one open, multi-domain codebase and a ground station that doubles as a full-stack lab. From rapid-prototype firmware to data-driven optimisation retainers, A-Bots.com shows how disciplined codecraft delivers measurable wins: 40 % fewer mission aborts, 70% faster surveys, and faster BVLOS approvals. Finally, the article looks ahead to AI-augmented navigation, Kubernetes-coordinated swarms and satellite-linked control channels, detailing the partnerships and R&D milestones that will shape autonomous, multi-domain operations through 2034. Read on to see why enterprises choose A-Bots.com to turn ambitious flight plans into certified, revenue-earning reality.
Otter Transcription and Otter Recording Otter.ai redefined speech intelligence; A-Bots.com makes it yours. We embed industry-leading otter transcription and otter recording directly inside purpose-built iOS, Android, and cross-platform apps, giving enterprises real-time captions under 450 ms, airtight on-device encryption, and adaptive language packs tuned to medical, legal, or industrial jargon. Our engineers design edge pipelines that thrive offline, orchestrate cloud bursts when GPUs add value, and wire finished transcripts into EHRs, CRMs, or analytics dashboards. Compliance? SOC-2, HIPAA, and GDPR controls ship in the very first build. Whether you need multilingual live captions for global webinars or secure voice logs for regulatory audits, A-Bots.com delivers a turnkey roadmap—from discovery to pilot to global rollout—so every conversation becomes structured, searchable intelligence that fuels growth.
GE Predix Platform Use Cases Across Industries This in-depth article maps nine high-impact industries where GE Predix delivers measurable ROI: power generation, upstream and midstream oil & gas, aviation engine health, rail freight, healthcare imaging, advanced manufacturing, water utilities, renewable microgrids, and smart buildings. You’ll learn how the platform’s digital twins, edge analytics, and zero-trust security cut downtime, energy spend, and carbon footprints, while A-Bots.com layers human-centric mobile apps that put those insights into the hands of engineers, traders, and CFOs alike. Perfect reading for decision-makers ready to unlock the full value of Industrial IoT with a proven development partner.
Top stories
Copyright © Alpha Systems LTD All rights reserved.
Made with ❤️ by A-BOTS
